They bring back early-life strategies, altering cell behavior in ways that accelerate growth.
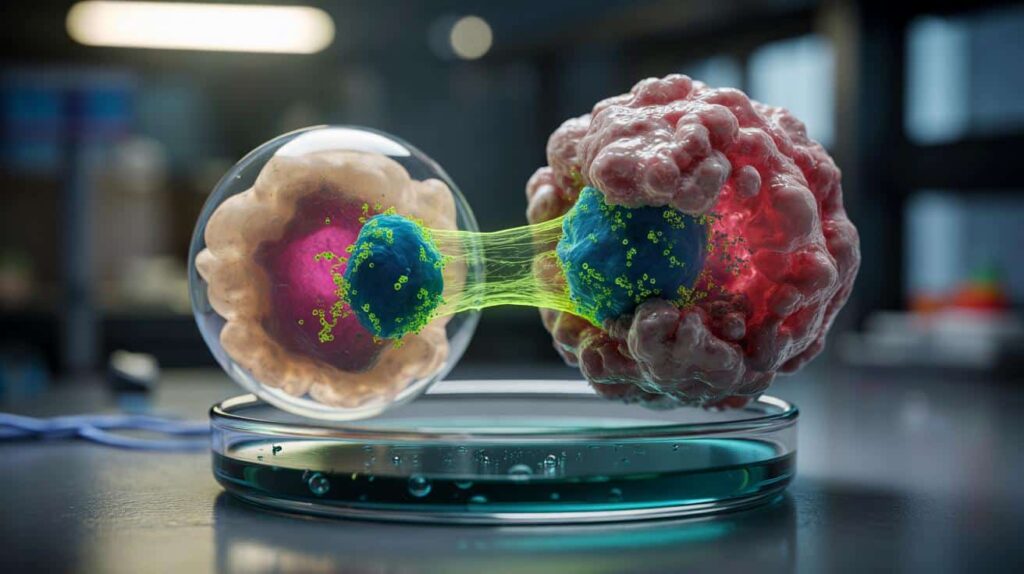
Recent research from European teams uncovers a concealed layer of control within malignant cells. Rather than rewriting DNA, cancer frequently modifies how gene messages are processed. This subtle adjustment, rooted in embryonic frameworks, enables tumors to divide more rapidly, adapt under stress, and evade treatment pressures.
A developmental switch turned back on
Researchers at the Centre for Genomic Regulation in Barcelona, in collaboration with ETH Zurich, report that many cancers reactivate molecular tools utilized during embryogenesis. These tools shape how RNA messages are processed, a crucial step that determines which protein variants a cell ultimately produces. The finding, published in Nucleic Acids Research, reinterprets rapid tumor growth as a reversion to early, highly adaptable states rather than merely an accumulation of DNA errors.
During early development, cells divide rapidly while retaining the potential to become various tissues. Tumors appropriate that flexibility. They repurpose elements of developmental programs to hasten division, alter identity traits, and survive in harsh microenvironments low in oxygen or nutrients.
Instead of creating new circuits, cancer reactivates old ones. The trick lies in how gene messages are interpreted and modified, not in the DNA sequence itself.
Why splicing is important
After a gene is transcribed, its RNA comprises segments known as exons and introns. Splicing eliminates introns and connects exons together. Alternative splicing rearranges exons in various combinations, producing diverse protein isoforms from a single gene. Cells rely on this adaptability to respond to signals, stress, and developmental cues.
Specialized proteins known as splicing factors regulate this process. In healthy tissues, their activity is finely tuned. The study indicates that cancers can reset that tuning to favor isoforms that promote proliferation, migration, and cell survival.
Splicing factors, repurposed for speed
The teams discovered that cancers revive a set of splicing factors typically active in embryos. A few “initiators” seem sufficient to shift the entire network. Since these proteins regulate one another, a small nudge can trigger a cascading change across hundreds of RNA decisions.
Change the editors, change the message. The genome remains unchanged; the output varies.
- Proliferation: isoforms that shorten the cell cycle gain prominence.
- Migration: transcripts favor traits associated with invasion and metastasis.
- Survival: pro-apoptotic variants decrease, while pro-survival ones increase.
- Therapy response: altered isoforms can obscure drug targets or pathways.
This cascade may go unnoticed by standard genomic tests. Sequencing the DNA might appear unremarkable, while the RNA layer has undergone significant changes. This discrepancy helps clarify aggressive behavior in tumors with relatively modest mutation loads.
The MYC footprint
The study emphasizes a well-known driver: MYC. This transcription factor regulates extensive gene programs related to growth and metabolism. When MYC is abnormally elevated, it enhances a select group of splicing-factor genes. These initiators then disrupt the broader splicing network.
This mechanism functions like an amplifier. MYC nudges a few nodes; the network amplifies the effect. A cell can transition from normal to malignant behavior without catastrophic DNA alterations. The outcome is a consistent, profound reprogramming of cell identity and pace.
A self-amplifying network
Splicing control resembles a complex web. Factors bind to shared RNA motifs, regulate each other’s expression, and create feedback loops. Disrupt one hub and ripples propagate. This interconnectivity poses a risk for tumors. It suggests that targeting a central node could restore balance across many miswired connections.
A minimal nudge at the right point could unravel a broad malignant program. This makes splicing hubs appealing drug targets.
From maps to medicine
To trace this hidden circuitry, the team trained an AI model on extensive transcriptome datasets. The tool infers which splicing factors are active based on bulk gene-expression patterns, avoiding the need to reconstruct every edited RNA molecule sample by sample.
Such readouts could serve as early biomarkers. Subtle changes in splicing-factor activity might manifest before a lesion is visible on imaging or before DNA mutations accumulate to detectable levels. In principle, these signatures could be assessed from tissue biopsies or blood-based tests that capture tumor RNA fragments.
| Feature | DNA mutations | Splicing reprogramming |
|---|---|---|
| Primary change | Modifies gene sequence | Modifies message processing |
| Speed of effect | Depends on mutation rate | Rapid, network-driven |
| Detectability | Standard genomics | Transcriptome-level signals |
| Therapeutic angle | Target mutated proteins | Target RNA editors and isoforms |
Therapeutic approaches
Targeting splicing does not imply editing DNA. It involves reducing specific factors, blocking their interactions, or directing the splice toward healthier isoforms. Given the interconnected nature of the network, a single precise intervention could produce significant effects. This raises the potential for lower doses and fewer side effects compared to broad cytotoxic drugs.
However, there are caveats. Splicing is crucial in normal tissues, including blood and brain. Drugs must spare essential programs while disabling tumor-specific rewiring. Patient selection will be important. A tumor with a distinct MYC-splicing signature may respond differently than one driven by alternative pathways.
Consider it as language therapy for cells: not rewriting the book, but teaching the editor to cut different paragraphs.
Implications for patients and laboratories
Clinicians could soon incorporate splicing signatures into decision-making tools, alongside mutation panels and protein markers. Anomalies may indicate aggressive disease even when imaging appears stable. In screening contexts, early splicing changes might signal increasing risk in tissues susceptible to malignancy.
For researchers and pharmaceutical companies, the map offers new leverage points. Inhibitors that modulate the spliceosome are already under investigation in early studies. Combining a splicing modulator with a MYC-pathway agent, or with drugs targeting metabolism, may prevent tumors from utilizing their embryonic shortcuts. Timing and sequence will be crucial, as these networks adapt rapidly.
Key concepts to understand
- Oncofetal programs: gene and RNA patterns active in embryos that reemerge in tumors.
- Alternative splicing: a process that generates distinct protein isoforms from a single gene.
- MYC: a growth-regulating transcription factor that can trigger splicing-factor cascades.
- Biomarkers: measurable signals, such as splicing activity, that indicate disease state.
Next steps to monitor
Two areas appear particularly promising. First, liquid biopsies that track splicing-derived RNA fragments could provide earlier alerts and real-time monitoring of therapy responses. Second, precision drugs that target a few splicing hubs may reset extensive tumor behavior with minimal exposure.
A practical exercise for readers: envision a tumor that depends on one embryonic splicing factor to sustain a pro-growth isoform of a metabolic enzyme. If a drug shifts splicing back toward the adult isoform, the tumor’s fuel supply tightens. Combining that shift with a modest dose of a metabolic inhibitor could weaken the cell’s safety net. This type of two-step strategy could minimize toxicity while targeting cancer where it leverages the past to influence its future.